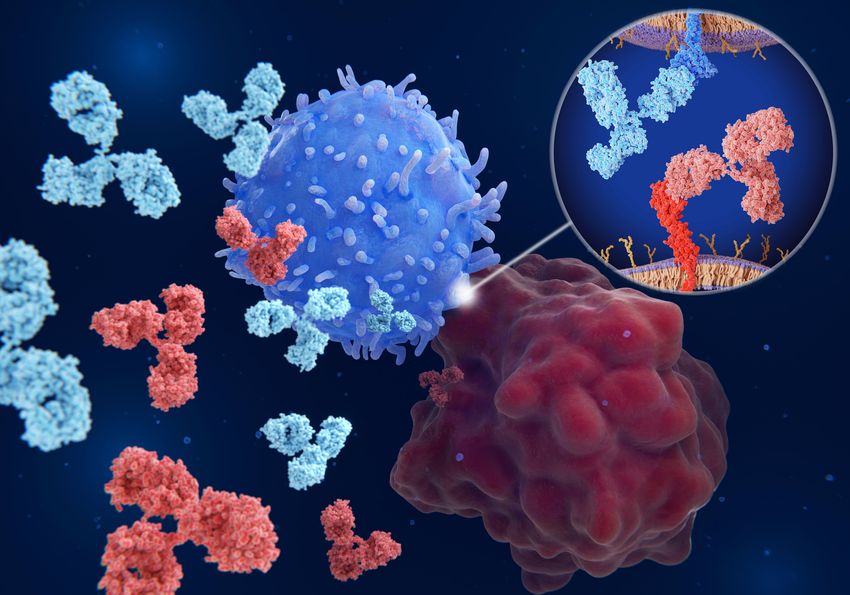
Cancer cells evade detection and destruction by modulating immune checkpoint signaling. Targeting these pathways to restore immune function can be an effective anticancer approach.
©iStock, selvanegra
Immune system activation and activity is regulated through stimulatory or inhibitory ligand-receptor interactions collectively termed immune checkpoints.1 Stimulatory interactions give the immune system the ability to identify and eliminate internal and external threats, while inhibitory interactions are instrumental in limiting autoimmunity and maintaining self-tolerance. Tumor cells, however, can modulate immune checkpoint signaling to promote their own survival, co-opting these signaling pathways to escape immune surveillance or shut down effector immune cell functionality.2
Recognizing this, scientists are looking for ways to reverse this phenomenon and restore or improve the immune system’s anticancer capabilities. Effector T cells play the most important role in anticancer responses, so researchers have focused most of their efforts towards looking at immune checkpoint interactions that regulate T cell activity.2 The spotlight has shone on two receptors in particular: programmed cell death 1 (PD-1) and cytotoxic T lymphocyte antigen 4 (CTLA-4).2,3 Both of these receptors mediate inhibitory mechanisms. CTLA-4 signaling dampens T cell activation while promoting regulatory T cell-mediated immunosuppression. PD-1 signaling limits T cell activity in peripheral tissues, ostensibly to limit autoimmunity and restrain inflammation.2
Immune Checkpoint Signaling and Immunotherapy
Checkpoint inhibitors, small molecules designed to block immune checkpoint ligand-receptor interactions, have been used clinically since 2011.3,4 These approaches have been approved for a wide variety of cancer types, including skin, colorectal, lung, kidney, and bladder.5 Unfortunately, the response rate has been lower than anticipated, hovering between 10-30 percent.6 More importantly, predicting which patients will or will not respond has been challenging, as responsiveness is governed by many factors, including tumor mutational burden, checkpoint expression levels, and cytokine signaling.5
Furthermore, checkpoint signaling modulates more than just T cell activation and the immune response at large. Researchers have shown that immune checkpoint pathways affect both T cell and cancer cell metabolism.7 For example, PD-1 and CTLA-4 signaling both inhibit glycolysis in effector T cells, leading to exhaustion and anergy. Glycolysis inhibition and the subsequent shift to fatty acid oxidation also promote the differentiation of memory T cells at the expense of effector counterparts. Accordingly, stimulatory checkpoint pathways promote glucose and mitochondrial metabolism, leading to elevated proliferation and effector function.7 Checkpoint signaling also affects cancer cell bioenergetics. Blockade of PD-L1 signaling, for example, leads to decreased glycolysis in tumor cells and increased lipid peroxidation leading to ferroptosis.7
Fittingly, scientists have studied how diet and caloric intake affects checkpoint inhibitor therapy response rate. The negative link between obesity and cancer progression is well established. However, obese metastatic melanoma patients treated with targeted checkpoint inhibitors paradoxically showed improved survival compared to non-obese counterparts. This result further aligns with murine model data showing augmented treatment effects in obese mice compared to lean.7 As such, researchers are looking into the prospect of using anti-diabetic agents such as metformin alongside checkpoint inhibitors as a combination therapeutic approach against cancer, with mixed results thus far.7
The Tools to Tackle Checkpoint Signaling’s Complexity
Immune checkpoint inhibitors hold great promise as anticancer therapeutic agents. It is clear though that immune checkpoint signaling is more complex and multifaceted than originally thought, and more research on how these signaling pathways operate during physiological and pathological conditions is necessary.
Companies such as Sino Biological support scientists in this endeavor by providing a comprehensive portfolio of recombinant immune checkpoint protein reagents, including co-stimulatory and co-inhibitory agents across multiple model species for binding assays, drug discovery, immunotherapy research, and more. These high-purity reagents are verified by HPLC and SDS-PAGE, and their bioactivity is validated using multiple techniques such as ELISA, surface plasmon resonance, and bio-layer interferometry. Furthermore, Sino Biological offers custom recombinant protein expression services for more personalized research goals.
